Understand your prescription options using the TRICARE Formulary Search Tool
The TRICARE Formulary Search Tool is an online resource that offers information about your TRICARE Pharmacy Benefit. It includes details on covered medications, copayments for TRICARE Home Delivery and in-network retail pharmacies, and forms for requesting Prior Authorization or Medical Necessity. This tool helps you better understand your prescription medication coverage, enabling you to make informed choices about your medication therapy.
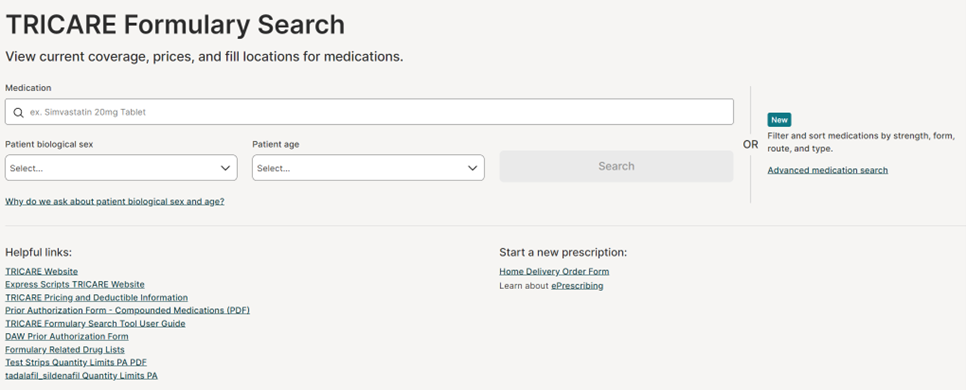
How to use the online tool
To get started, visit the TRICARE Formulary Search Tool. To initiate a search, enter either the brand name or the generic name of the medication and select the strength from the options in the drop-down menu. Additionally, you will need to select your biological sex and age. It is important to choose the correct age and biological sex as the search results will provide coverage information specific to those factors. For more details on how to use the tool, refer to the TRICARE Formulary Search Tool User Guide under the ‘Helpful links’ section.
Filter and sort medications by strength, form, route, and type by using the Advanced medication search option.
What a medication search will show you
- If the medication can be filled at a military pharmacy, TRICARE Home Delivery, or an in-network retail pharmacy, and applicable copayments.
- General information about the medication including what it is used for, medication images, alternate names, and frequently asked questions.
- Coverage results and requirements, and forms needed to process the prescription such as Prior Authorization and Medical Necessity forms.
- Quantity and day supply limits.
- Alternative medication options.
Where to fill your prescriptions
Military Pharmacy
You can get up to a 90-day supply of most medications at military pharmacies. Medications are free of cost when filled at a military pharmacy. Find a military pharmacy near you by visiting tricare.mil/mtf.
TRICARE Home Delivery
With home delivery, you can receive up to a 90-day supply of most maintenance medications along with free standard delivery (copayments apply). It is easy to manage your medication routine using automatic refills and the free Express Scripts® Pharmacy mobile app.
In-Network Retail Pharmacies
At in-network retail pharmacies1, you can get up to a 30-day supply of your medication. The TRICARE pharmacy network gives you access to convenient in-network retail pharmacy locations throughout the U.S. and its territories. Find a Pharmacy near you.
For more information visit the helpful links section under the search bar at www.esrx.com/tform.
If you have additional questions about your prescription medication coverage, contact us at 1-877-363-1303.
Published 6/6/2025.
- 1
At non-network retail pharmacies, beneficiaries will pay full price for their prescriptions. Beneficiaries can file a claim for reimbursement. Reimbursements are subject to deductible or out-of-network cost-shares, and copayments. All deductibles must be met before TRICARE can reimburse.